There is emerging evidence for, and good evidence for risk reduction, such as life style changes as a way of preventing a diagnosis of dementia. It is, for me and many others living beyond dementia, in spite of the sector telling us to go home and give up, very exciting times!
There is emerging evidence for, and good evidence for risk reduction, such as life style changes as a way of preventing a diagnosis of dementia. It is, for me and many others living beyond dementia, in spite of the sector telling us to go home and give up, very exciting times!
Common sense certainly says to me, that we must also take the same approach for someone who is diagnosed with dementia, and start to use non pharmacological and positive psychosocial interventions for dementia immediately upon diagnosis.
Who knows how many of us could possibly even stay at work, with immediate and intensive rehabilitation, in the same way we would have been supported to if we’d had a stroke or any other brain injury?!
When I was first diagnosed, and for some time after, I almost accepted the Prescribed Disengagement® dished up to me. Thank goodness i didn’t and it mostly thanks to being at university, and being directed to their disAbility Advisors, I found another way to live with dementia
One with support for disAbilities, and a focus on the assets I still had, rather than simply being told to go home and die. I then decided to think about it with my ‘nurses hat’ on, and wondered why I had not been offered intensive rehabilitation. It seemed logical to me, and in reality, it was unethical not to have been offered support to live with dementia.
Luckily for me, I continued to study at university, which I believe is one of the keys to my slower deterioration of symptoms. Not meaningless brain training games on an iPad, but really interesting courses that stretch me to think really hard, pushed me to find ways to write, stretching my brain to learn new things, which quite often these days, I don’t remember, but that is not the point.
For me, studying something I am really interested in is a truly engaging, meaningful and purposeful activity, and excellent neuroplasticity training. So much more fun than Bingo…
There are three books I consider more than recommended reading for anyone who wants to change their life, their thinking, and improve their health, as follows.
Norman Doidge’s book The Brain That Changes Itself, offers significant anecdotal evidence we can rewire our brain. I firmly believe that. Dr Bruce Lipton’s book The Biology of Belief: Unleashing the Power of Consciousness, Matter and Miracles, brings evidence to light that it is possible to change your cells through belief. I also believe that, and have since my early 20’s. Dr Lipton has proven it. And finally, Dr Martin Seligman’s book Flourish: A Visionary New Understanding of Happiness and Well-being is on changing our thinking, and flourishing by being more positive. I met him a few years ago, and told him he had stolen my manuscript! When I read this book, I felt as if I had written many parts of it, as I have been on that path also since my 20’s.
I have written and presented many times on the non pharmacological and positive psychosocial interventions I use to live beyond dementia. They may not be a cure. Many of them have little evidence (yet) to support them. However, they do ensure my life is more positive, meaningfully engaging, and productive. For me, they are the Olympics of my life.
Earlier this year, I was talking to Professor Dimity Pond, an academic general practitioner from NSW about some of the interventions I use, and after some of her own research into the value of speech pathology for dementia, she said;
“It was very interesting talking to you about the speech therapy rehabilitation around word finding and so on which you have found so helpful. I have done some reading around this over the weekend and can see that there may be a sound biological basis for it.
Of course you are right that there are other non pharmacological interventions that are helpful as well.”
I was delighted she took me seriously, and did some research into it, as she is currently involved in writing guidelines for dementia. This blog is a list of the interventions I was engaging in back in 2013, which has been revised and added to significantly since then.
My physical rehabilitation includes almost daily brisk walking for 60 minutes, Pilates, strength and balance exercises, speech pathology, hydrotherapy, as well as Transcendental Meditation, Mindfulness, and self-hypnosis for pain management. The reason for the last two, is that I live with high levels of chronic pain, and do not like the cognitive side effects of medication stronger than paracetamol, and so, only very occasionally take anything for pain.
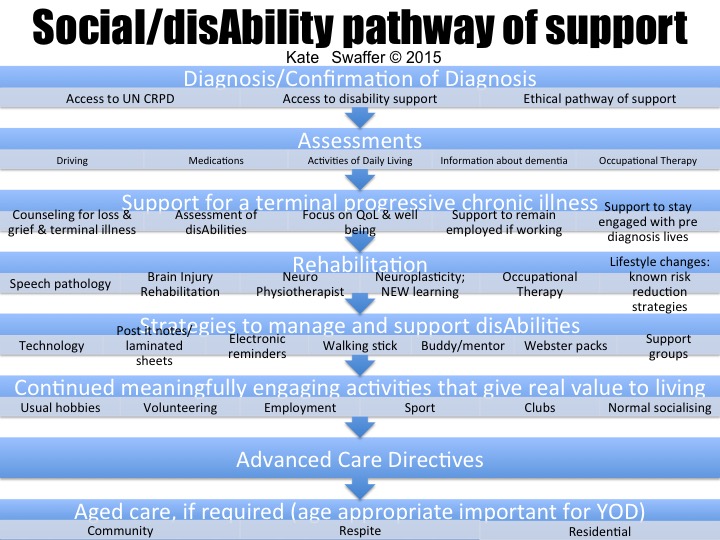
The slide above is of the ‘Social/disAbility Pathway of Support’ I have been working on for many years, and used recently at a Better Practice conference in Brisbane. Feel free to use it, referencing it to me – but also please let me know if you do, as I do like to know where my work or words end up. As I work on it further, I will also add more about it here as well.
We really must find ways to improve the post diagnostic pathway of dementia care, at least in line with someone who has had a stroke, and I am delighted there are one or two professionals working on this as well now. Thank you.
Finally, Advocacy is one of the positive psychosocial and non pharmacological interventions for dementia that I use, almost daily, and when I look around the world at who is living beyond dementia, and who is speaking out and advocating, they are often the very same group.
I strongly recommend speaking out, and up, for yourself, especially if you have dementia. Do not let people without dementia dictate what is best for you, nor tell you how you feel.
Of course, there are quite a few feathers being ruffled globally, feathers belonging to people without dementia, who do not seem to like their position of power and supposed knowledge about our experience, being challenged. That’s ok, I’ll keep speaking up for what I believe to be a more ethical pathway of support for all people with dementia.
Recommended reading:
Doidge, N, 2012, The Brain That Changes Itself, Scribe Publications.
Lipton, B, 2005, The Biology of Belief: Unleashing the Power of Consciousness, Matter and Miracles, Hay House Inc. (This is much cheaper bought as a Kindle book)
Seligman, M, 2011, Flourish: A Visionary New Understanding of Happiness and Well-being, Free Press.
 I’ve not been blogging much lately, barely monthly here, and certainly not daily on my other blog like I used to. I suppose though, it is good to report the reason why is I am actually too busy living beyond dementia to have the time!
I’ve not been blogging much lately, barely monthly here, and certainly not daily on my other blog like I used to. I suppose though, it is good to report the reason why is I am actually too busy living beyond dementia to have the time!


 One would have to say, I am managing to live beyond dementia, and alongside of it, in spite of the
One would have to say, I am managing to live beyond dementia, and alongside of it, in spite of the  Whilst I have not been publishing each day on my
Whilst I have not been publishing each day on my  There is emerging evidence for, and good evidence for risk reduction, such as life style changes as a way of preventing a diagnosis of dementia. It is, for me and many others living beyond dementia, in spite of the sector telling us to go home and give up, very exciting times!
There is emerging evidence for, and good evidence for risk reduction, such as life style changes as a way of preventing a diagnosis of dementia. It is, for me and many others living beyond dementia, in spite of the sector telling us to go home and give up, very exciting times!